A 60 year old female with SOB, facial puffiness and decreased urinary output
23/10/2022
Student Name- D.Vineesha Chowdary
2017 batch
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHIEF COMPLAINTS-
A 60 year old female presented to the casualty with chief complaints of - Urinary urgency since 30 days- fever associated with chills and rigor 20 days ago for 3 days - decreased urinary output since 15 days- cough since 15 days- breathlessness since 1 day- facial puffiness since 1 day
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic twenty days ago when she developed high grade fever associated with chills and rigor for 3 days that was intermittent in type and relieved on taking medication. She also has urinary urgency since 30 days and decreased urinary output since 15 days. She also had cough that was productive, non foul smelling, non blood stained since 15 days. Since one day she also has facial puffiness and breathlessness and the patient sought for consultation at a local hospital and was started on diuretics and was discharged on LAMA.
PAST HISTORY-
Patient has a history of bilateral knee pain since 5 years and was prescribed ointment and NSAIDS.
Patient is a known case of hypertension since 6 months.
FAMILY HISTORY-
No significant family history
PERSONAL HISTORY-
Appetite- lost since 2 months
Diet- Mixed
Bowel movements- normal
Bladder movements- Burning micturition, decreased urinary output, urinary urgency
Sleep- adequate
Any addictions- 1 glass of toddy since 40 years twice a week, and betel leaf daily since 40 years.
Any allergies- No
GENERAL EXAMINATION-
Done after obtaining consent, in the presence of attendant with adequate exposure
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is well nourished and moderately built.
Vitals-
On 22/11/22
Temperature- 97.8F
Blood pressure- 110/70 mmHg
Pulse rate- 78 bp
Respiratory rate- 18 cpm
SpO2- 98%
Pallor- Absent
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Edema- presentABDOMINAL EXAMINATION-
INSPECTION- Umbilicus inverted , No abdominal distention, no visible pulsations, scars and swelling.
PALPATION- Soft, non tender, no organomegaly.
AUSCULTATION- Bowel sounds heard
CVS EXAMINATION-
INSPECTION- No visible pulsations, scars, engorged veins. Rise in JVP present.
PALPATION- Apex beat is felt at 5th Intercoastal space medial to mid clavicular line.
AUSCULTATION- S1, S2 heard, no murmurs.
RESPIRATORY SYSTEM-
INSPECTION- Shape of chest is elliptical, b/l symmetrical.
PALPATION- Trachea is central. Expansion of chest is symmetrical.
Bilateral Airway Entry - positive
AUSCULTATION- Normal vesicular breath sounds.
Rhonchi present.
CNS EXAMINATION-
No signs of meningeal signs
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++ ++
Triceps. + +
Supinator + +
Knee. ++ ++
Ankle - -
Gait: normal.
INVESTIGATIONS-
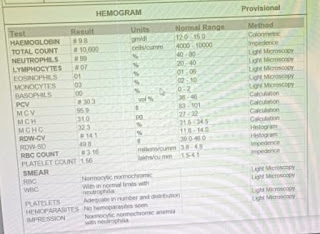
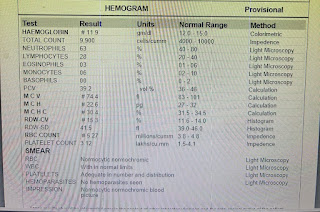
HAEMOGRAM-
S.CREATININE-
S.CALCIUM-
S.PHOSPHOROUS-
CUE-
USG
2D ECHO
CHEST X RAY-
ABG-
PROVISIONAL DIAGNOSIS-
AKI SECONDARY TO SEPSIS AND K/C/O HTN
TREATMENT-
1) IVF NS/RL @75ML/HR
2) FOLEYS CATHETERIZATION
3) INJ.NEOMOL (if temp > 101F)
4) INJ.PAN 40 MG/IV/OD
5) INJ.ZOFER 4MG/IV/SOS
6) INJ.PIPTAZ 2.5GM/IV/TID
7) NEB. DUOLIN 6TH HRLY
8) NEB.BUDECORT 8TH HRLY
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is well nourished and moderately built.
Temperature- 97.8F
Blood pressure- 110/70 mmHg
Pulse rate- 78 bp
Respiratory rate- 18 cpm
SpO2- 98%
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Edema- present
ABDOMINAL EXAMINATION-
INSPECTION- Umbilicus inverted , No abdominal distention, no visible pulsations, scars and swelling.
PALPATION- Soft, non tender, no organomegaly.
AUSCULTATION- Bowel sounds heard
CVS EXAMINATION-
INSPECTION- No visible pulsations, scars, engorged veins. Rise in JVP present.
PALPATION- Apex beat is felt at 5th Intercoastal space medial to mid clavicular line.
AUSCULTATION- S1, S2 heard, no murmurs.
RESPIRATORY SYSTEM-
INSPECTION- Shape of chest is elliptical, b/l symmetrical.
PALPATION- Trachea is central. Expansion of chest is symmetrical.
Bilateral Airway Entry - positive
AUSCULTATION- Normal vesicular breath sounds.
Rhonchi present.
CNS EXAMINATION-
No signs of meningeal signs
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++ ++
Triceps. + +
Supinator + +
Knee. ++ ++
Ankle - -
Gait: normal.
INVESTIGATIONS-
HAEMOGRAM-
S.CREATININE-
S.PHOSPHOROUS-
CUE-
USG
2D ECHO
CHEST X RAY-
ABG-
PROVISIONAL DIAGNOSIS-
AKI SECONDARY TO SEPSIS AND K/C/O HTN
TREATMENT-
1) IVF NS/RL @75ML/HR
2) FOLEYS CATHETERIZATION
3) INJ.NEOMOL (if temp > 101F)
4) INJ.PAN 40 MG/IV/OD
5) INJ.ZOFER 4MG/IV/SOS
6) INJ.PIPTAZ 2.5GM/IV/TID
7) NEB. DUOLIN 6TH HRLY
8) NEB.BUDECORT 8TH HRLY








Comments
Post a Comment