67 year old patient with acute coronary syndrome
May 14,2021
Student Name- D.Vineesha Chowdary
2017 batch
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
HISTORY OF PRESENTING ILLNESS:
A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2 hour.
She had H/O heartburn like episodes since a year. They were relived without use of any medication.
She has H/O TB diagnosed 7 months ago for which she completed the course of medication a month ago.
Patient was apparently asymptomatic till 9pm on that day (27/4/21). She apparently ate dinner and slept. When she woke up at night for washroom she developed sweating on exertion and shortness of breath even at rest.
No H/O chest pain, palpitations, giddiness, nausea, vomiting, LOC, pedal oedema, decrease in urine output,PND.
No H/O fever, cough, cold, sore throat.
PAST HISTORY:
K/C/O of DM2 since 12 years and is on Rx GLIMI M2 PO/BD
K/C/O of hypertension since 6 months and is on Rx TELMA 20 mg PO/OD
H/O pulmonary TB 7 months ago when she had cough, chest pain. Completed the course for TB a month ago. Currently negative for TB.
FAMILY HISTORY:
No significant family history
PERSONAL HISTORY:
She had mixed diet with normal appetite,
Adequate sleep,
Regular bowel and bladder movements
And no addictions.
EXAMINATION:
On examination, the patient was conscious, co-operative, coherent.
Patient was oriented to time, place and person.
VITALS: ( Upon admission)
BP- 130/80 mm Hg
PR- 126 BPM
Afebrile
CVS- S1, S2 +, no murmurs
Respiration- B/L, Inspiratory crepts +, dyspnoec
Sp O2- 96%
GRBS- 256 Mg/dl
P/A- Soft, Bowel sounds +
CNS- NAD
INVESTIGATIONS-
1) An ECG was done upon admission. The ECG shows NSTEMI ( acute coronary syndrome)
An ECG will show the following characteristics for an NSTEMI:
- depressed ST wave or T-wave inversion
- no progression to Q wave
- partial blockage of the coronary artery
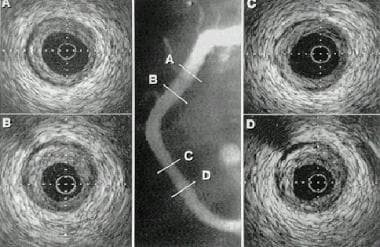
2) A chest X-Ray was taken in another hospital on the next day.
3) A chest CT scan was taken in another hospital the following day.
PROVISIONAL DIAGNOSIS- Acute coronary syndrome (NSTEMI)
Treatment at hospital-
Upon seeing the ECG, the patient was given TAB MET XL 25 MG/STAT.
The patient was then advised to shift to a HC for PCI upon explaining to the patient’s attender about the patient’s condition.
The patient was then taken to another hospital, for further treatment but PCI was not done as there were no vacancies in hospitals at that time.
The patient was discharged after that and is currently doing fine.
DETAILS ABOUT PCI:




Comments
Post a Comment