Student Name- D.Vineesha Chowdary
2017 batch
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 80 year old female came to casualty with complaints of shortness of breath and chest pain since 2pm on (25/3/22)
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 years ago when she developed giddiness. She was diagnosed as hypertensive then and was given medications (Amlodipine 5mg, atenolol 50mg).
Patient had generalized weakness since 3 days that was associated with sob which is grade II.
Then yesterday at around 2pm, she developed shortness of breath which is grade IV(while at rest) for which she went to local hospital and was given some medications after which the symptoms subsided. At around 8pm she again developed SOB (grade IV) in association with chest pain and came to our casualty.
Patients SpO2 was 40@Ra
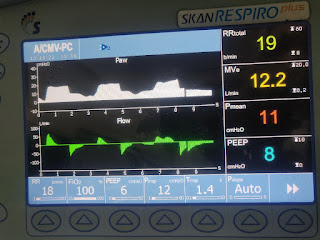
In the view the patient was intubated at below settings.
After intubation, the patient went into cardiac arrest, pulse was week and BP was non recordable. Then 3 cycles of CPR were done along with adrenaline (1ml per each cycle of CPR).
PAST HISTORY:
She was diagnosed with hypertension 3 years ago and was on medication.
FAMILY HISTORY:
No significant family history
PERSONAL HISTORY:
She had mixed diet with normal appetite,
Adequate sleep,
Regular bowel and bladder movements
And no addictions.
EXAMINATION:
Vitals on admission:
PR: 90bpm
BP: 90/60 mm hg@norad6ml/hr, dobutamine 5ml/hr)
SpO2: 40% on RA
Cvs-s1s2 +
Rs-BAE+
P/a- soft
On examination,
Mild pallor present.
No icterus, cyanosis, clubbing, lymphadenopathy.
INVESTIGATIONS-
Post intubation ECG:
Yesterday at 7am:
26/03/22
ABG at 12:30pm
ABG at 7am:
RBS, RFT, LFT, trop i:
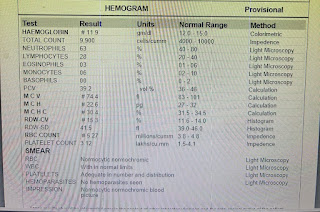
Hemogram:
Serology - negative
Diagnosis:
? Unstable angina
?acute exacerbation of COPD
Patient intubated 26/3/22 at 1:30am post CPR status 3 cycles.
Treatment: Day 1
1) inj.norad - 2amp in 46ml ns @6ml/hr.
2) inj dobutamine - 1amp in 45ml ns @5ml/hr
3) inj.Clexane - 60mg/sc/bd
4) tab.ecospirin 325/RT/stat
5) tab.clopidogrel 200mg/rt/stat
6) tab.atorvastatin 80mg/rt/stat
7) bp monitoring hrly
8)inj.NaHCo3 50mg/iv/stat
Day 2
1) Rt feeds 100ml milk and 10ml water @4th hrly
2) inj.augmentin 1.2gm/iv/bd
3) inj.norad - 2amp in 50ml ns @20ml/hr.
4) inj dobutamine - 1amp in 50ml ns @5ml/hr
5) inj.vasopressin (1amp + 50ml NS) IV @2ml/hr
6) inj.heparin 5000IU /IV/QID
7) tab.ecospirin 150mg/RT/stat
8) tab.clopidogrel 200mg/rt/stat
9) tab.atorvastatin 40mg/rt/OD
10) Nebulisation with budecort and mucomist @8th hrly
11) vitals monitoring hrly
12) frequent post change every hrly
13) arterial and central line every 4th hrly
14) strict I/o charting
Update- 27/03/22
At around 12 pm patient’s central pulses were absent with refractory hypotension and falling saturations due to which CPR was initiated according to 2020 AHA guidelines.
In spite of 7 cycles of CPR the patient couldn’t be revived and was declared dead at 12:35 pm.
Immediate cause of death-
- coronary artery disease
- acute left ventricular failure with pulmonary oedema
- refractory metabolic acidosis
- refractory hypotension













Comments
Post a Comment