Student Name- D.Vineesha Chowdary
2017 Batch
Roll no.- 24
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CHIEF COMPLAINTS:
A 48 year old male came to the OPD on 17th may with chief complaints of
Fever since 7days,
Dry cough since 5 days,
Difficulty of breathing since 5 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic until 7 days ago when he developed-
-Fever which was insidious in onset, intermittent in nature, not associated with chills and rigor.
-Dry cough which was insidious in onset, intermittent in nature with no positional or diurnal variations. No aggravating and relieving factors were noted.
-He developed Grade 2 SOB 5 days ago, insidious in onset and gradual in progression.
-No complaints of chest pain, vomiting.
-No loss of smell and taste.
PAST HISTORY:
Not a k/c/o hypertension or diabetes.
FAMILY HISTORY:
-No history of similar complaints in the family.
-No history of DM, TB, Stroke, Asthma, or any other hereditary diseases in the family.
DRUG HISTORY:
No significant drug history.
PERSONAL HISTORY:
Appetite: Normal
Diet: Mixed
Bowel movements: Regular
Bladder movements: Normal
No known allergies
No addictions
GENERAL EXAMINATION:
The patient is examined in a well lit room with informed consent.
The patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is moderately built and well nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS:
On 17/5/21 (At the time of admission):
Temperature- Afebrile
Heart Rate- 82BPM
Blood pressure- 110/60 mm of Hg
Respiratory rate- 20/min
SPO2- 89% at room air
GRBS- 127 mg/dl
On 18/5/21:
Temperature- Afebrile
Heart Rate- 78BPM
Blood Pressure- 110/70 mm of Hg
SPO2- 96% at 6L of O2
On 19/5/21:
Temperature- Afebrile
Heart Rate- 84 BPM
Blood Pressure- 110/70 mm of Hg
SPO2- 90% at room air
95% at 4L of O2
On 20/5/21:
Temperature- Afebrile
Heart Rate- 96BPM
Blood Pressure- 110/70 mm of Hg
SPO2- 91% at room air
96% at 10L of O2
GRBS- 186 mg/dl
On 21/5/21:
Temperature- Afebrile
Heart Rate- 82 BPM
Blood Pressure- 110/80 mm of Hg
SPO2- 93% at room air
SYSTEMIC EXAMINATION:
CVS SYSTEM: S1,S2 heard
No added thrills, no murmurs
RESPIRATORY SYSTEM:
Dyspnea: Grade 2 SOB
Wheeze: Absent
Position of trachea: Central
Breath sounds: Vesicular breath sounds heard
Adventitious sounds: Not heard
PER ABDOMEN:
Soft, non tender, no organomegaly
CNS:
Intact
INVESTIGATIONS:
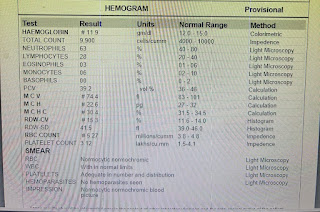
Complete Blood Picture:
On 17/5/21:
On 20/5/21:
ABG:
ECG REPORT:
PROVISIONAL DIAGNOSIS:
Viral Pneumonia secondary to COVID-19 and DM.
TREATMENT:
During the stay in the hospital-
- O2 inhalation to maintain SPO2 > 90%
- TAB PAN 40 p/o OD
- Nebulisation (8 hourly)
- SYP ASCORIL LS 10 ml TID
- TAB DOLO 650 p/o /SOS
- TAB MVT p/o OD
- TAB LIMCEE p/o OD
- Incentive Spirometry
- T.P.R B.P charting 4 hourly
- GRBS 6th hourly
- Inj HAI according to GRBS
- Tab AUGMENTIN 625 mg p/o BD
- Inj CLEXANE 40 mg SC OD
- Inj DEXAMETHASONE 6mg IV OD
- Monitor temperature, PR, BP, SPO2
Advice on discharge-
- O2 inhalation if SPO2 < 90% at room air
- TAB AUGMENTIN 625 mg p/o BD for 1 week
- TAB PAN 40 mg p/o OD for 1 week
- TAB MVT p/o OD for 1 week
- TAB LIMCEE p/o OD for 1 week
- TAB DOLO 650 mg p/o SOS
- SYP. ASCORIL LS 10 ml p/o TID for 1 week
- INJ. CLEXANE 40mg SC OD for 1 week
- INJ. DEXAMETHASONE 8 mg IV OD for 1 week
- INJ. HAI according to GRBS
8 am 1 pm 8 pm
- GRBS monitoring 6th hourly at home
-INCENTIVE SPIROMETRY
- TAB GLIMI M1 p/o 1-0-0 to continue
Patient was discharged on 20/05/21
Vitals at time of Discharge:
Temperature: Afebrile
Heart rate: 86 BPM
Blood pressure: 120/60 mm of hg
SPO2: 95% on room air
Under the guidance of Dr. Sai Charan sir







Comments
Post a Comment