Student Name- D.Vineesha Chowdary
2017 batch
Hall ticket number- 1701006034
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Following is my view of the case:
71 year old male with shortness of breath and cough with expectoration
CHIEF COMPLAINTS-
A 71 yr old man presented to the OPD with chief complaints of:
- Shortness of breath since 25 days.
- Cough with sputum since 25 days
- Fever since 9 days.
HISTORY OF PRESENTING ILLNESS-
-Patient was apparently asymptomatic 25 days ago when he developed Grade 2-3 shortness of breath, that was aggravated on exertion, exposure to cold air, relieved by rest. It was insidious in onset. It was associated with wheeze. No history of orthopnea or PND.
-Cough with expectoration was non foul smelling, non blood stained. Sputum was mucoid. It increased during nights. No postural variations. It was relieved on taking medications.
-Fever was low grade, continuous. No evening rise of temperature, not associated with chills. It was relieved on medication.
-There was loss of appetite and weight.
PAST HISTORY-
No history of pulmonary TB or covid 19 in the past.
No similar complaints in the past.
Not a k/c/o Diabetes mellitus, Hypertension, CAD, Epilepsy.
FAMILY HISTORY-
No history of similar complaints in the family.
No history of DM, TB, Stroke, Asthma, or any other hereditary diseases in the family.
TREATMENT HISTORY-
Not on any medications.
PERSONAL HISTORY-
Appetite: reduced
Diet: Mixed
Bowel movements: Regular
Bladder movements: Normal
Sleep: Adequate
No known allergies
History of smoking- 50 pack years.
No other addictions.
GENERAL EXAMINATION-
The patient is examined in a well lit room with informed consent.
The patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is thin built and malnourished.
Weight- 34kg
Pallor: Present
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS-
On 02/06/22:
Heart Rate- 102 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 26/min
SPO2- 90% at room air
On 03/06/22:
Heart Rate- 89 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 26/min
SPO2- 96% at room air
On 04/06/22:
Heart Rate- 94 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 92% at room air
Temperature-98.4F
On 05/06/22:
Heart Rate- 90 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 96% at room air
On 06/06/22:
Heart Rate- 88 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 22/min
SPO2- 98% at room air
On 07/06/22:
Heart Rate- 92 BPM
Blood Pressure- 120/80 mm of Hg
Respiratory rate- 24/min
SPO2- 91% at room air
SYSTEMIC EXAMINATION-
CVS SYSTEM: S1,S2 heard
No added thrills, no murmurs
RESPIRATORY SYSTEM:
Dyspnea: Present
Wheeze: Present
Position of trachea: Shifted to right
Inspection-
Shape of chest-B/L symmetrical, elliptical.
Chest movements decreased on right side.
No kyphosis, or scoliosis.
No crowding of ribs.
No scars, sinuses, visible pulsations or engorged veins.
No wasting of muscles
No usage of accessory muscles.
Palpation-
All inspectory findings are confirmed.
Trachea shifted to right side.
No local rise of temp.
Chest movements decreased on right side.
Percussion-
Right side ICA impaired note
Right SSA impaired
TVF equal on BS.
Auscultation-
Vesicular breath sounds
Right SSA + LSA decreased breath sounds
Right MA crepts +ve.
PER ABDOMEN:
Soft, non tender, no organomegaly
CNS: Intact
INVESTIGATIONS-
ECG-
2D ECHO-
HRCT of Thorax-
Other investigations done-
PFT
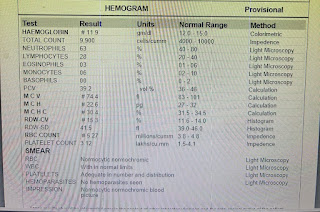
CBP
CUE
LFT
RFT
ECG
PROVISIONAL DIAGNOSIS-
Right Upper lobe fibrosis
On 1/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
On 2/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
On 3/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
On 4/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
On 5/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
Needle thoracocentesis-
Done under aseptic conditions. Done under the guidance of USG. Betadine was painted at 5th ICS on right side, mid clavicular line. 2% Xylocaine was instilled and a 20CC syringe was inserted and pleural fluid was aspirated of about 20ml which was straw colored. Procedure was uneventful.
Post procedure vitals-
PR- 100BPM
BP- 120/80mmhg
RR- 24CPM
spO2- 94% @ RA
On 6/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Inj. OPYINEURON IV
Tab. ACECLO-TH BD
On 7/6/22-
Tab. AUGMENTIN 1.2gm IV TID
Tab. PAN 40mg OD
Tab. PCM 650mg BD
Syrup ASCORIL-LS 2Tbsp
Neb. with BUDECORT BD
DOULIN TID
MUCOMAL TID
O2 inhalation with nasal prongs @ 2-4L/min
Maintain spO2 > 94%
Tab. AZEE 500mg OD
Syrup CREMAFFIN 10ml HS
Tab. ACECLO-TH BD
Diclofenac patch






Comments
Post a Comment