Student Name- D.Vineesha Chowdary 2017 batch
Hall ticket number- 1701006034
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
70 year old male with weakness of right upper and lower limbs
Following is my view of the case:
CHIEF COMPLAINTS-
A 70 yr old man presented to the OPD on 06/06/22 with chief complaints of:
- Weakness of right upper and lower limb since 3 days.
- Slurring of speech since 3 days
- Drooling of saliva since 3 days.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 3 years ago when he developed sudden onset weakness of right upper and lower limbs, without slurring of speech. After being treated, he then recovered from it. After 2 years (a year ago) he developed a second episode of sudden onset weakness of right upper and lower limbs, that was associated with drooping of mouth, drooling of saliva, slurring of speech. He was again treated for it and recovered completely. He then had a third episode of sudden onset weakness of right upper and lower limbs 4 days ago. He also had drooping of mouth on one side, drooling of saliva, slurring of speech associated with right sided weakness of the limbs.
No history of involuntary movements, urinary incontinence.
No history of nausea and vomiting.
No h/o head injury, up rolling of eye balls.
PAST HISTORY-
Patient is a k/c/o hypertension since 1 year and is on regular medications (Tab. Atenolol 25mg).
Patient is not a k/c/o diabetes mellitus, TB, epilepsy, asthma.
FAMILY HISTORY-
No history of similar complaints in the family.
No history of DM, TB, Stroke, Asthma, or any other hereditary diseases in the family.
TREATMENT HISTORY-
On medication for hypertension (Tab. Atenolol 25mg).
PERSONAL HISTORY-
Appetite: Normal
Diet: Mixed
Bowel movements: Regular
Bladder movements: Normal
Sleep: Adequate
No known allergies
History of alcohol addiction that stopped 5 years ago.
No other addictions.
GENERAL EXAMINATION-
The patient is examined in a well lit room with informed consent.
The patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is moderately built and well nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
VITALS-
On 06/06/22 (At the time of admission):
Temperature- Afebrile
Heart Rate- 70 BPM
Blood Pressure- 140/80 mm of Hg
Respiratory rate- 16/min
SPO2- 98% at room air
On 07/06/22:
Temperature- Afebrile
Heart Rate- 80 BPM
Blood Pressure- 130/80 mm of Hg
FBS- 158mg/dl
GRBS- 167mg/dl
SYSTEMIC EXAMINATION-
CVS SYSTEM: S1,S2 heard
No added thrills, no murmurs
RESPIRATORY SYSTEM:
Dyspnea: Absent
Wheeze: Absent
Position of trachea: Central
Breath sounds: Vesicular breath sounds heard
Adventitious sounds: Not heard
PER ABDOMEN:
Soft, non tender, no organomegaly
CNS:
Patient is conscious/alert.
Speech-slurred
No signs of meningeal irritation
Cranial nerves- NAD
Sensory system- NAD
Motor system-
Right Left
Tone- UL Decreased Normal
LL Decreased Normal
Power- UL 0/5 4/5
LL 0/5 4/5
REFLEXES-
Biceps- +++ ++
Triceps- +++ ++
Supinator- +++ ++
Knee- +++ ++
Ankle- +++ ++
Blood group- A+ve
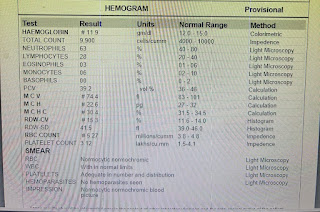
Hemogram-
Hb%- 12.6gm/dl
TLC- 8,600 cells/cumm3
RBC- 4.33million cells
Neutrophils- 55%
lymphocytes- 35%
Eosinophils- 03%
Blood Urea- 24mg/dl
Serum creatinine- 1.3mg/dl
Serum electrolytes-
Sodium- 136mEq/L
Potassium- 3.7mEq/L
Chloride- 104mEq/L
LFT-
Total bilirubin- 0.61mg/dl
Direct bilirubin- 0.16mg/dl
SGPT- 11 units/L
SGOT- 13 units/L
Alkaline phosphate- 105 IU/L
Albumin- 4g/dl
A/G Ratio- 1.71
PT- 2min
ECG-
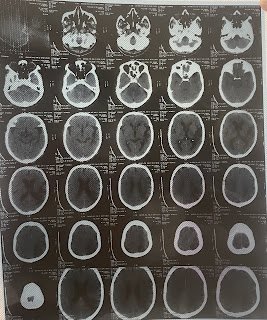
CT scan-
Present-
1yr ago-
PROVISIONAL DIAGNOSIS-
Acute ischemic stroke causing right sided hemiplegia (left MCA territory)
Recurrent CVA
TREATMENT-
Tab Ecospirin 150mg PO OD
Tab Clopidogrel 75mg PO OD
Tab Atorvas 40mg PO HS
Tab Pan 40mg PO OD
Tab Aten 25mg PO OD
Physiotherapy of right upper and lower limbs
Monitoring vitals





Comments
Post a Comment