A 68 year old male with altered sensorium
June 26 2021
Student Name- D.Vineesha Chowdary
2017 Batch
Roll no.- 24
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 68 year old Male with altered sensorium
Following is the view of my case:
CHIEF COMPLAINTS:
Patient presented to the casualty in an altered state with GCS E4V1M4
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic until one and a half hour ago when he was going for a nature call and was made to sit on a chair and then he suddenly became altered with a history of fall.
There was history of deviation of mouth to right
No history of involuntary movements, urinary incontinence.
No history of nausea and vomiting.
No h/o head injury,Uprolling of eye balls
No h/o post ictal confusion
PAST HISTORY:
K/C/O Asthma since 14 years and on MDI
K/C/O HTN since 7 years and on amlong.
K/C/O of CVA in august 2020 with MCA ischaemic infarct with unresolved AF and with inferior wall MI.
Not a k/c/o Type 2 diabetes, TB.
FAMILY HISTORY:
No history of similar complaints in the family.
DRUG HISTORY:
T.Amlong 2.5mg PO OD for HTN.
T Amiodarone 150mg PO BD
PERSONAL HISTORY:
VITALS:
RT SIDED
biceps 3+ , triceps 1+ ,supinator 1+,knee 3+, ankle 2+
LT SIDED
biceps 3+, triceps 3+ , supinator 3+ , knee 3+, ankle 2+
No cerebellar signs
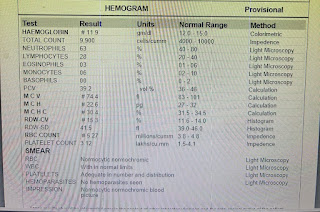
INVESTIGATIONS:
1) Serum electrolytes
2) Serum creatinine
3) Blood urea
-Tab Nicardia 10mg PO stat
-Tab Ecosporin 150mg PO h/s
-Tab clopitab 75mg PO h/s
-Tab Amlong 2.5mg PO OD
-Tab Atorvas 40 mg PO h/s
-BP charting 4th hourly
On 25/6/21:
-Tab ecosporin 75mg PO
-Inj optineuron 1 ampoule in 100 ml NS OD
-Tab atorvas 40 mg PO
-Tab clopidogrel 75 mg PO
-Tab amlong 2.5mg PO OD
- BP charting 4th hourly
-SYP potchlor 10ml PO BD
-Tab amiodarone 150mg PO BD
Discontinued from the last 4 years







Comments
Post a Comment